Dr. Allison McConnell
Program Director
amccon2@uwo.ca

Dr. Brendan Maxwell
Assistant Program Director
rmaxwel3@uwo.ca

Susan Pierson
Program Administrator
susan.pierson@lhsc.on.ca
Program Overview
Interested in chatting with us about our program? Reach out to our PGY-3 Medical Student Liaisons at westernemergmed@gmail.com!
Western is a medium sized Emergency Medicine program situated in London, Ontario with a large catchment area. We have 3 hospitals and are a level 1 trauma centre with a full compliment of clinical services and resources. We have an incredibly engaged group of residents and faculty, and provide an excellent training experience in a supportive environment. Please read through the rest of the information for further specifics. We always welcome connection from those interested in learning more about our program and London, as we are proud of the education and experience our residents get here.
The residency at Western traditionally consisted of a five year, 65 block curriculum with a rough breakdown of one-half EM related rotations, and one-half off-service rotations, including medicine, surgical and trauma specialties, critical care environments, psychiatry, toxicology, and EMS/Pre-hospital care. The residency also supports longitudinal experiences in research, and other areas of special interest such as; Fellowships in POCUS, EMS/pre-hospital care, critical care, resuscitation, and sports medicine, and Masters Programs in medical education, epidemiology and biostatistics, public health, trauma, and disaster planning, and business administration.
The residency has now transformed into a competency by design curriculum. The first four residents started in the CBME model in July 2018. This allows residents to traverse a wide range of medical specialties as they progress from an introductory stage to transition to EM practice. Western will continue to graduate the next generation of stellar EM clinicians who will be well equipped to practice in the ever-changing and increasingly complex environment of
academic Emergency Medicine.
Quick Facts:
- There are four core learning sites which include University hospital, Victoria hospital, Children’s hospital which are all a part of London Health Sciences Centre. University hospital is our Cardiac and Neurology centre, while Victoria Hospital is our trauma, Psychiatry, and Obstetrical and Gynecology site. In Addition, our Urgent Care Centre at St. Joseph’s hospital is a location that the residents rotate through regularly which also boasts our Hand and Upper Limb Clinic and Ophthalmology.
- We have opportunities to work out our distributed sites including St. Thomas, Stratford, Strathroy, Woodstock, Chatham, Windsor etc. Our catchment area is large, providing significant opportunity to be exposed to a wide breadth of pathology and diverse populations. Our Obstetrics rotation is done in Windsor as a PGY2 and is a satellite site for our undergraduate Medical students as well.
- There are currently 22 residents (4-5 per year) in the Emergency Medicine Residency Program spanning 5 clinical years. Currently there are 90+ faculty members at The London Health Sciences Centre and 16 full-time Pediatric Emergency physicians at the Children’s Hospital of Western Ontario and additional locums.
- It is very common for residents to take electives in Clinical Toxicology at The Hospital for Sick Children in Toronto and also at Bellevue Hospital in New York City (NYCPC) Although these are by definition electives, the program currently supports residents for travel and accommodation.
- There are many other electives that have been undertaken, and the program is always thrilled to support new endeavors.
- Our program is currently making some significant changes to incorporate our community stakeholders and agencies into our education and training. This is in its early stages, but hope to have more regular teaching and involvement with local agencies that serve our various patient populations. In turn, this will provide us with the opportunity to have some additional elective potential in social medicine and with our underserved populations, and more discussion and teaching around EDI topics. We have a new addictions service and elective that began in 2022-2023 academic year, and are looking for further expansion of these opportunities on a more formal basis. We are committed to expanding our incorporation and celebration of diversity into all aspects of our program.
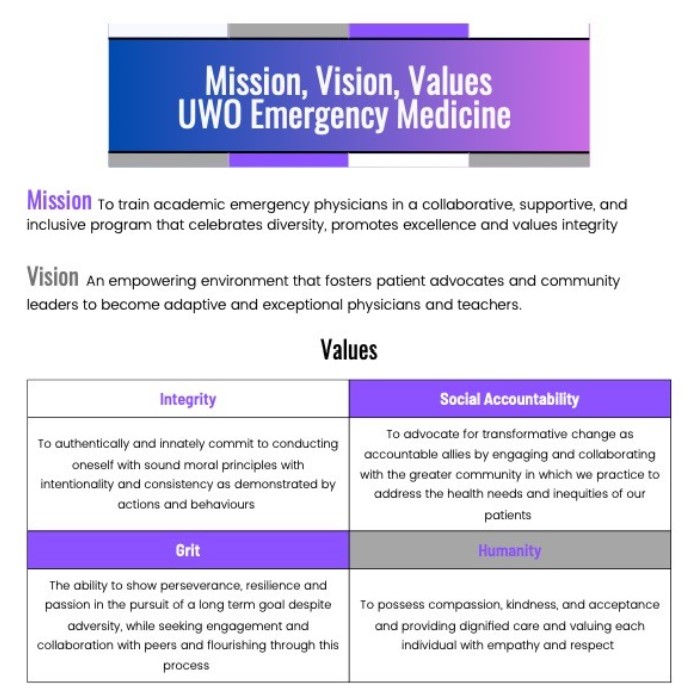
The Emergency Medicine program at Western endeavors to provide an environment in which we work together, residents and faculty to flourish under any circumstances to help our patients, all of our colleagues and our community. We have recently drafted a new Mission, Vision and Values outlined below. As a group we have identified the ideals and characteristics of our program, and where we would like to strive to be. These qualities will guide our selection criteria, endeavoring to engage more students to build and support our effort to work together to build a better program, department and community.
Curriculum
Year ONE: Transition to Discipline and Foundations
- Adult ER (4)
- UCC (1)
- Paeds ER (2)
- Anesthesia (1)
- POCUS/EMS (1)
- CTU (1)
- Gen Sx (1)
- Psych (1)
- Paeds Gen Sx (1)
Year TWO: Core
- Ortho Trauma (1)
- Ortho Hybrid – urgent care shifts with a focus on ortho presentations (1)
- CCTC (ICU) (2)
- Cardiac critical care unit (2)
- Anesthesia (1)
- Adult ER (4)
- Paeds ER (1)
- OB/Gyn (1) – Windsor
Year THREE: Core
- ER SMR (1)
- Trauma (1)
- Paediatric CCU* (2)
- Adult ER (4)
- Paeds ER (2)
- Electives (2)
- Neuro (1/2 stroke; ½ community clinic)
*One PCCU block may be substituted for paeds transport
Year FOUR: Core
- Adult ER (5)
- Paeds ER (2)
- UCC (1)
- Electives (5)
Year FIVE: Transition to Practice
- Area of interest (6)
- Electives (2)
- ER (5)
During electives in 3rd year and 4th year, residents must complete EMS, Advanced POCUS, and Toxicology rotations
The strengths of the program reside within the dedicated faculty, the commitment to teaching, and the extensive and varied patient population and catchment area. We are constantly looking to improve and expand our curriculum, and have a rotation of evaluating each aspect of the program, as well as regular input from the residents longitudinally to assure we are meeting the requirement of the Royal College/accreditation, as well as the needs of our learners and faculty. Our faculty are engaged and enthusiastic, as are our residents.
Quarterly we review 2-4 rotations formally at our RPC meetings, and adjust these learning opportunities accordingly. We are in the process of adapting our objectives and target EPAs for each of these rotations to ensure there is clear competencies, EPAs and objectives associated with each rotation.
Residents are evaluated on a quarterly by means of direct observation and in-training examinations, both written and oral in nature, EPAs, clinical mentors, presentation and teaching evaluations, Simulation, and research. The Program Director and Competence Committee review resident progress on a regular basis and feedback is regularly provided. We are currently working with our PGME for their upcoming improvements in our online EPA system to further this ability.
Academic days
Each Thursday we have our protected academic teaching day. These run from September to June, and July and August are “summer school” (see below).
8am – Senior resident rounds
9am – Grand Rounds
10-12 – Core Rosen’s teaching
1pm – afternoons sessions (varied, see below)
Our senior resident rounds are organized by our PGY5 residents and consist of some clinical pearls, quizzes, games and guest speakers. Our accredited Grand Rounds is a 1 hour session conducted by faculty, a combination of faculty and residents or outside guest speakers spanning a variety of topics. These are in person, and a welcome return to this format after COVID.
Our Core Rosen’s teaching is 2 hours, and has recently been reorganized to be on a 3 year rotation to cover all the topics in the new 10th Edition. Faculty are required to teach around the topic as per the Rosen’s chapter, but also include relevant literature, guidelines, an example of an oral case and written exam, as well as case based teaching. The information is then stored in a secure online database for the residents to access after. The expectations prior to the teaching include reviewing the Rosen’s chapter and objectives and literature or material provided by the faculty conducting that session. These sessions have the expectation to be done in a psychologically safe fashion, with an awareness to EDI principles and information surrounding effective teaching in a didactic fashion, as well as an awareness to planetary health in this context.
In the afternoon there is monthly high fidelity simulation that is held at another facility for all of the FRCPC residents. We have recently renovated part of our Emergency medicine space to accommodate a small simulation lab at the hospital, and look to expand the Simulation time in the 2024-2025 year. Other simulation sessions include other procedural days including canthotomies, open thoracotomies, tendon repairs, cricothyrotomy on cadavers in our anatomy lab. Our PGY2s also have a comprehensive curriculum for their sports medicine/ortho hybrid rotation with intermittent sessions dedicated to the musculoskeletal exam and management of these injuries and conditions.
There is also an afternoon each month that is dedicated research time, the residents have this free to use for research if they choose. There is no scheduled session during this time.
The other afternoons are a new addition as of the 2023-2024 academic year. These include varied medico-legal topics, communication, teaching as a resident, evolution of learning and studying, how to combine in person and virtual learning, learning strategies, geriatrics additional teaching, pediatric dental teaching, social medicine and engagement, leadership, styles of learners, clinical epidemiology, QA teaching, sessions from our local police surrounding human trafficking, 2SLGBTQ+ session and subsequent simulation session, indigenous sensitivity training and are working on additional sessions surrounding trauma informed care, trans health, and around our role in helping our under privileged and under served patients.
These afternoons also allow us to enjoy team building and wellness activities as a group.
We have an annual Airway Day, which includes extensive teaching from our local airway experts (including some AIME instructors), Anesthesiologists and Critical Care Physicians. We also have a Resident Research day annually to allow both the FRCPC and CCFP-EM and medical students to present their research.
In addition, we have quarterly confidential Human Rounds with the PD. These were a safe space for residents to discuss the more difficult aspects of medicine and residency in a supportive group of peers. This is open to any aspect of life or residency that they want to discuss, and is completely voluntary. We are looking to expand these in this upcoming year.
Summer School
During July and August our Thursday teaching is organized differently, and includes orientation and ice breaker sessions for the PGY1s, an introductory POCUS course and EMS orientation and introductory Simulation sessions for the PGY1 cohort, and this is often paired with the CCFP-EM residents. The sessions during the rest of the summer include increased focus on procedures (lines, chest tubes, casting, nerve blocks, surgical airways, pericardiocentesis etc), trauma, critical care, blood gas interpretation, EPA/CBME updates, toxicology, plastics pearls, and wellness activities.
Exam Preparation
We have a study schedule that residents can use and modify that is provided, as well as mentorship from previous residents and faculty. With this there is formal written and oral exams performed throughout the year, as well as informal oral exams and written exams performed before or after shifts, and on other time. Our faculty is very engaged in this preparation. Should a resident have some difficult, a learning plan and additional mentorship and supervision is established if needed. Regular communication with the residents studying the PD/APD, RPC and faculty facilitate studying and mentorship throughout this challenging year. There is a shift reduction in the several months prior to the exam, and further during exam months. Our PGY4 and 5 residents self schedule with specified guidelines to facilitate exam preparation and their AFC/AFI in their PGY5 year.
Transition to Practice
The 2022-2023 year was the first year we had a transition to practice (T2P) cohort. They had some separate teaching with further detail about medico-legal teaching, litigation, financial transition to faculty, how to disclose errors, becoming a teacher as a faculty, and legislation and complaint processes. In addition, they had a dedicated simulation day revolving around transition to practice content. They were expected and welcomed to additional teaching roles for both postgraduate, undergraduate students, undergraduate coaching, death review committee, additional CaRMS opportunities, oral exam development and administration, learner supervision and simulation teaching. There was the ability to alter rotations and shifts based around future practice and perceived need, and support throughout to assure all aspects of clinical and non-clinical objectives were addressed. We also had the opportunity to have a T2P block which allowed the residents to focus on department flow and organization, supervision of learners, documentation, handover, billing, receiving patch calls, addressing the nursing concerns and close oversight of clinical plans. These were identified to faculty, and particular competencies were focused on in each shift with a discrete evaluation associated with this. The T2P residents enjoyed these. This was also in addition to an optional “teaching” block if the residents wanted to focus their teaching together.
Area of Focused Competency/Interest and Fellowship
We have had a variety of interests and here at UWO have a formally accredited PoCUS and Prehospital AFC program, as well as being a centre with a Pediatric Emergency department with the opportunity for further pursuits of Pediatric Emergency Medicine. Other pursuits have included Critical Care, Trauma, Toxicology, Resuscitation and Reanimation/Simulation, Medical Education, Addictions, Research, Clinical Epidemiology, Masters in Health Administration, Masters in Business Administration, Masters in Public Health, Narrative Medicine, Wilderness Medicine, Sports Medicine, Palliative Care and more. The opportunities are extensive and well supported by our program. We are able to individualize the T2P year, and time throughout residency to suit each resident’s particular needs and desires.
Journal Club
Our journal club was significantly disrupted by COVID, and is the rebuilding stage. This year likely will see each portfolio do a dedicated journal club (ie Simulation, PoCUS, Preshopital, Wilderness, FRCPC, CCFP-EM). These have been in the evening and are accompanied by a meal. The 2024-2025 year has plans to have some additional changes as our Research program evolves.
In addition to journal club, we have “Bottom lines” sessions which are organized by our chief residents and supervised by some of our research faculty. These comprise of a collection of practice changing papers, both historical and recent. Each resident is tasked with summarizing 1-2 articles both written and orally, and then these are shared with the group.
Mentorship and Feedback
Each resident is provided with 2-4 clinical mentors whom they work with in each Emerg block throughout residency. These are based on both clinical, research and other non-clinical interests, and can be altered or added to as things evolve. In addition, each resident has a longitudinal Competency Committee (CC) mentor who is in touch at least quarterly, and often more frequently.
The PD and APD meet biannually with each resident individually, and frequently if desired/requested or necessary for any reason. The PD/APD, CC and Residency Program Committee (RPC) members as well as other faculty and chief residents are very readily available should urgent issues arise.
Our CC meet quarterly followed by our RPC to review EPAs, clinical mentor feedback, block evaluations, teaching evaluations, research progress, CITE (Canadian In Training Exam) results, oral exam results, Simulation evaluation, Grand rounds/other presentation evaluations. This is then fed back to the resident for their review, and pre and post meeting the residents are asked for input and feedback. The residents are also invited to the RPC meetings, and there is a senior and junior representative present at each RPC meeting.
Should a resident require extra learning, we have the ability to support the with faculty and resident mentorship and learning plans. If a resident is exceeding expectations, we are also able to adjust the opportunities to meet these learners needs as well.
Resident Research Opportunities
Each trainee is expected to be involved in one scholarly project at all times. Although this may involve research, residents are also encouraged to be involved in the planning, implementation and evaluation of educational programs as well as continuous quality improvement projects, development of guidelines and care pathways and disseminating this work. Ideally, these scholarly activities are of long-term interest. Residents are expected to present their work annually at the program’s Residents Research Day, and have substantial support from our research office and mentors. Presentations may include a completed project, or a description of a project that is currently being designed, or a progress report of a long-term project.
We have a faculty member who is designated as resident research coordinator, however most faculty members are involved in research either through their role on the research committee or as individual project supervisors. Our research coordinators work in the research office and are excellent resources for project design and clinical epidemiology. They also deliver clinical epidemiology teaching sessions throughout the year during Thursday morning chief rounds.
Resident Research Day (RRD)
Resident Research Day (RRD) is an annual event held in the spring by the emergency medicine department. Here, residents from both the royal college and CCFP-EM programs present their active research projects. In order to encourage quality work, residents may present project proposals, work in progress, or completed work. It is expected that each royal college resident will present at a minimum of three RRDs during their five-year residency. A group of judges, including a visiting physician from an external hospital, award monetary prizes to the best oral presentations.
National & International Conferences
Royal college residents are expected to present their research findings at a minimum of one national level conference during their residency. Most often, residents present at the annual Canadian Association of Emergency Physicians conference.
Selection Criteria
For full information regarding our file review and selection process, please see our information on the CaRMS website, which is updated annually.
In general, we are looking for:
- Proven interest in emergency medicine as demonstrated by enthusiasm in the interview, previous elective experience in emergency medicine, letters of reference from emergency physicians familiar with the candidate
- Commitment to an academic/scholastic practice of Emergency Medicine
- Excellent interpersonal skills
- An acceptable academic record
- Elective Requirements: We encourage applicants to have completed at least one elective in our specialty.
- On Site Elective: We do not require applicants to have done onsite electives.
As outlined by the file review process we look at candidates’ personal statement, scholarly activity, life experience, ability to demonstrate social accountability and references.
We value different applicants and strive for diversity in all aspects of our program, community involvement and education. We hope to see meaningful commitments and do not require quantity of activities but value quality and passion in these pursuits. We hope to see aspects of humanity, integrity, collaboration with leadership in difference capacities appreciated.
We strive to be an engaged, supportive environment that hold each other accountable while we build towards excellence as a group and individuals.
Resident Support
Residents are provided with a copy of the textbook Rosen’s Principles and Practices of Emergency Medicine at the beginning of their residency. In addition, residents receive $500.00 per year in academic funding to use towards conferences, textbooks or other academic uses. Residents who have projects accepted for presentation at national conferences receive an additional $1500.00 to offset the costs of travelling to the conference. Resident travel and accommodation costs for the toxicology and trauma electives are supported. The programs helps fund other recommended courses (PALS, Classic), and boots needed for EMS rotations as well as an annual resident retreat.
Training Sites
Clinical experience is gained at the London Health Sciences Centre which includes the Children’s Hospital of Western Ontario. The London Health Sciences Centre also operates as a regional Trauma Referral Centre. It is also the Base Hospital for the Prehospital Care Program. London has both Basic and Advanced Life paramedics in the field that are under on-line and off-line medical control. Rotations also occur at St. Joseph’s Health Centre which runs an urgent care center.
There are opportunities for interprovincial and international electives while training in the program. Past residents have done electives in other provinces in Canada, the United States and around the world. These electives need to be arranged by the residents with approval of the residency training committee. In general, there is not financial support for residents in these electives.
Electives
Undergraduate students may be interested in an elective in Emergency Medicine at UWO are welcomed! Now with the return of electives following COVID, the link is https://www.schulich.uwo.ca/medicine/undergraduate//md_program/visiting_student_electives.html
Medical students are required to apply through the AFMC portal.
If you are coming for an elective, please reach out as we would love to be able to introduce our program to you, and have you at our academic teaching days. If you are unable to get an elective we completely understand this is largely out of your control. We would still be happy to discuss the program with you. Please consider following us on Instagram @westernuemerg for updates and information on our virtual office hours with the residents. In addition our senior residents can provide additional contacts and information at westernemerg@gmail.com.
Previous Program Graduates
1985 David Austin, University of Toronto
Robert Beveridge, Dalhousie University
1987 Mary Eisenhauer, Western University
Rob Street, University of British Columbia
1988 John Gibson, Western University
1989 Lisa Shepherd, Western University
1990 Graham Bullock, Dalhousie University
Jeff Fuss, University of Victoria
1991 William McCauley, Western University
1992 David Murphy, Western University
1993 Pauline Paine, Western University
1995 George Kovacs, Dalhousie University
1996 Scott Anderson, Western University
David Petrie, Dalhousie University
1997 Karen Woolfrey, McMaster University
1998 Keith Donovan, Western University
Michael Hatcher, MacMaster University
1999 Derrick Pringle, Western University
2000 Michael Lewell, Western University
Dawn Giffin, Western University
2001 Phil Moran, North York General
2002 Drew Thompson, Western University
Andrew Jones, Western University
2003 Ted Everson, Western University
Terry Skoretz, Western University
2004 Laura Price, Western University
Colin Bullard, International
Jehangir Meer, University of Toronto
2005 Becca Mallin, McMaster University
Abdullah Al-Ghamdi, International
2006 Wanda Millard, Western University
2007 Ian Ball, Western University
Adam Dukelow, Western University
2008 Kris Lehnhardt, Washington
Mike Peddle, Western University
2009 Rob Arntfield, Western University
Dave Ouellette, Western University
2010 Chris Martin, Barrie, ON
Jan Trojanowski, Vancouver, BC
2011 Cimi Achiam, Vancouver BC
Karalyn Church, Western University
Heather Hames, Western University
2012 Matt Davis, Western University
Allie Meiwald, Western University
2013 Sameer Mal, Western University
Joel Krause, St. Catherines, ON
Ryan Arbeau, Western University
Danny Peterson, Calgary, AB
2014 Justin Yan, Western University
Justin Ahn, Vancouver, BC
2015 Bourke Tillmann, Toronto, ON
Morgan Riggan, Western University
Kate Hayman, Toronto, ON
2016 Natalie Cram, Calgary, AB
Sean Doran, Western University
Megan Garnett, Thunder Bay, ON
Chris Lee, Vancouver, BC
2017 Dave Fu, Edmonton, Alberta
Lauren Valdis, Western University
Ben Strauss, Credit Valley, Mississauga
2018 Allison McConnell, Western University
Jacob Pace, Western University, St Thomas
Drew Schappert, Western University
Marcus Van Aarsen, Western University
Meagan Mucciaccio Windsor Regional
Alex Dong, Western University
2019 Mike Beyea, Brampton ON
Nick Federman, Chatham/Guelph ON
Chantal Forristal, Western University
Marc Lipkus, North York, Toronto ON
Davy Tawadrous, Toronto General
2020 Michael Clemente, Western University
Mason Curtis, Western University
Aaron Stone, UBC
Brad Waterman, Western University
2021 Michael Blaszak, Windsor ON
Erik Leci, Western University
Jennifer McGuire, Western University
Brad Rostas, Western University
John Teefy, Western University
2022 Shane Freeman, Western University
Danielle Kelton, Western University
Brendan Maxwell, Western University
Dave Morden, Western University
Petrease Patton, Western University
2023 Taylor Beauchamp, Western University
Sydney Todorovich, Western University
Rob Soegtrop, Toronto ON
Erfun Hatam, Windsor ON
2024 Stephanie Chilton, Western University
Emily Oura, Western University
Daniel Korpal, Western University
John MacIsaac, Hamilton ON